The Complex Nature of Your Pain
Whether it's a running-related injury or otherwise, pain is highly complex when it is fresh and acute, and even more so when it has become chronic (> 3 months). That's because extent of tissue damage (and even just presence of tissue damage) doesn't directly equate to amount of pain. In fact, your experience of pain is made up of 3 contributors: the biological, the psychological and the social. That means that the biomedical component of pain (aka the actual structural damage or inflammation) is only 1/3 of the equation!
A Tale of Two Nails
A good way to exemplify the extent to which our brain contributes to pain is the tale of two nails. As the first story goes, a man steps on a board and sees a nail come up and through his boot. He immediately screams in pain and is brought to the hospital where they remove the boot to find no wound or blood. The nail went right between his toes
In the second scenario, a nail gun accidently discharges on a construction worker. He sees a nail sail by his head and lodge into the wall behind him, he experiences no pain. A few days later he has gone to the dentist over increasing jaw pain. The x-ray reveals a 4" nail that was embedded in his face.
The Biomedical Component - The Body
This is the variable we're all most familiar with when we think of why we have pain. When you sprain your ankle, the immediate tissue damage will create some pain response locally. If that ankle becomes swollen, the swelling in the joint can press on structures causing pain, or restrict motion which can indirectly lead to discomfort. Prolonged immobility leads to tightness and guarding and weakness which leads to poor movement patterns. All have the end result of contributing to pain in some way. Maybe this has now been a cycle going on 3+ months after your sprain and you've found yourself dealing with this cycle of pain.
For the majority of the history of medicine, these biomedical factors were where we've almost solely attempted to intervene. We've done so with orders to rest, pain medication, and physical therapy to help heal tissue. Yet research has shown that a little negative expectation can completely reverse the analgesic effect of an opioid. Similarly, the expectation of pain relief is the driving force behind the placebo effect. Yet another example of the brain being a driving force.
The Psychological Component - The Mind
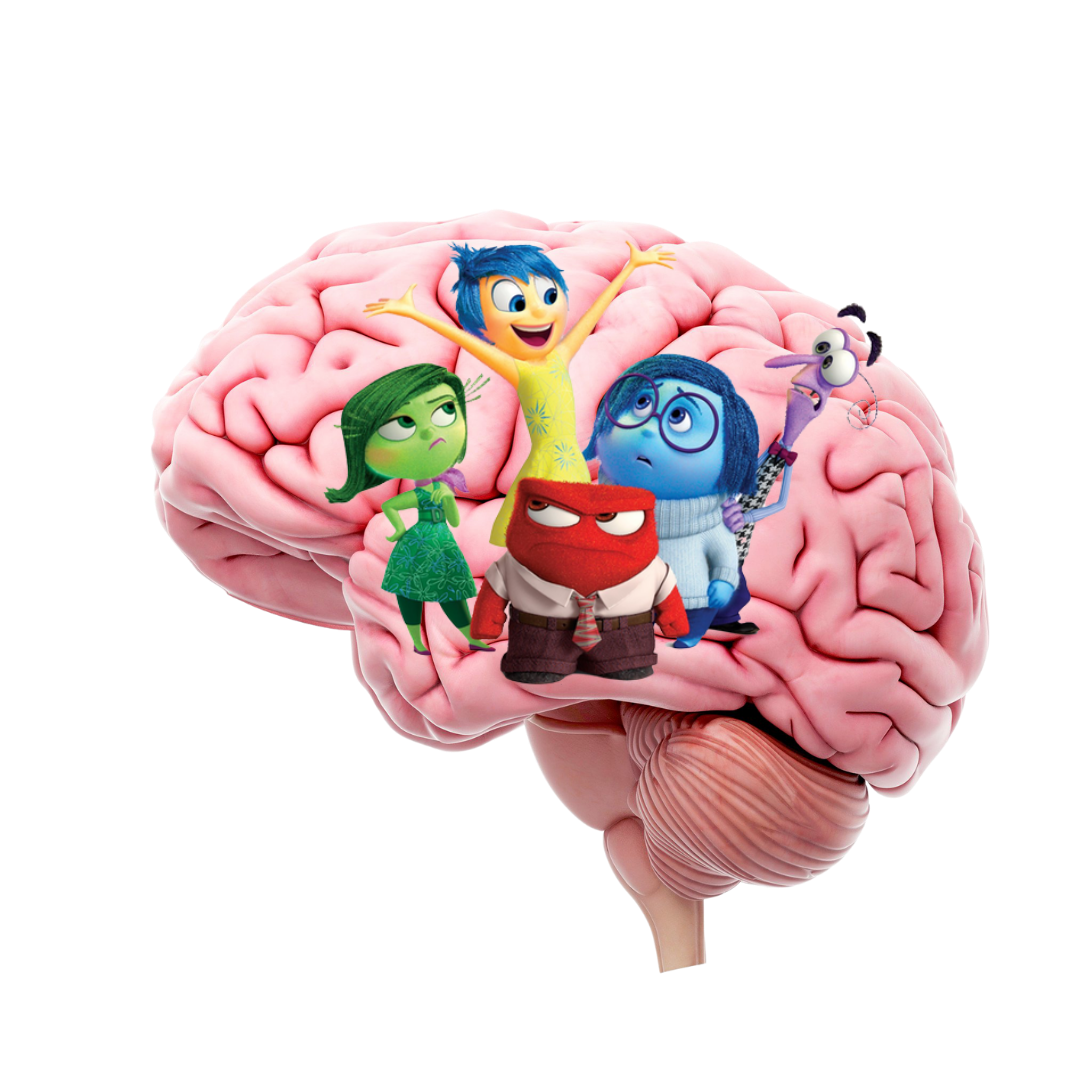
Pain is constructed by your by brain using all available information from the world and your body. It is our body's alarm system for danger, which is meant to help us, but has the tendency to misfire like in the tail of two nails. In this scenario, one man's brain identified danger (based on seeing a nail go through his shoe) and signaled pain to him without the presence of any actual tissue damage. Crazy, right? But also something we need to consider in modern medicine.
When it comes to pain, think of it as a dial that lives inside our central nervous system and can be turned up and down. This dial is heavily regulated by the limbic system which is responsible for behavioral and emotional responses related to survival. Things like high stress/anxiety or negative emotions like depression and anger all turn up the pain dial. The good news? We can use just the opposite to turn the dial on pain down.
The Sociological Component - The World
You've experienced the aforementioned ankle sprain but things have taken longer to heal than expected. You're 4-5 months out and still dealing with discomfort that has prevented you from confidently returning to run. Now the the extended immobility that lead to localized weakness has resulted in a lack of outlet for your stress and anxiety. It means you haven't been able to participate in your weekly run club which is your support system and primary social group. A lack of ability to engage in enjoyable activities leads to more tension which leads to more guarding and feelings of helplessness and more time to focus on your pain.
But here's the thing, at 4-5 months out that biomedical component (that ankle ligament) should be mostly healed. However, you've entered this pain cycle which has continued perpetuate a problem. You need a plan.
Breaking The Cycle
1. Recognize the Mental Piece
Take care of your mental health needs by finding outlets for stress relief.
Think positively about your recovery and recognize the role fear and negative outlook can play
2. Utilize Relaxation Strategies
Things like belly breathing and meditation lower the pain dial by relaxing the flight or fight system and affecting the limbic system
These strategies reduce muscular tension as well which eases pain by affecting the biomedical side as well
3. MOVE
If you're in the acute phase of injury, finding ways to move without irritation of the tissue promotes healing and teaches the brain that movement is OK
If you're at a chronic point where the source tissue has healed, it's important to start getting back to activity in a progressive way
Your brain needs to rewire and relearn that certain movements it previously identified as "dangerous" are safe
Getting back to physical activity triggers hormonal responses that improve mood and returning to previous social engagements around activity distracts from pain
Chronic pain is complex and it's vital we understand the multi-dimensional nature of it to help you get back being active. If you're having a hard time getting back to running or doing what you love please reach out to discuss what's missing in your current approach!